
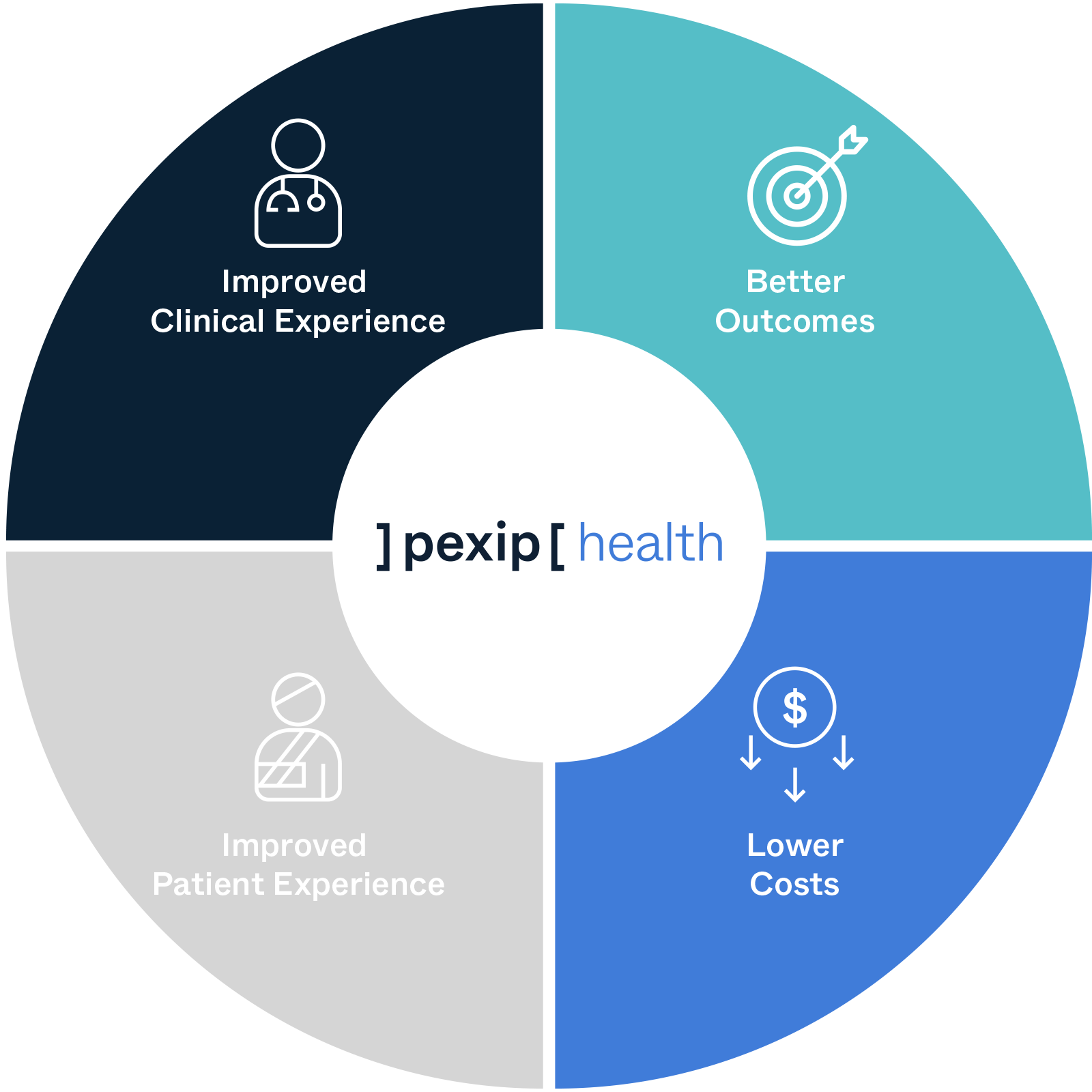
Last August AHRMM released a CQO report based on the clinically integrated supply chain. Thus, the Triple Aim should expand to the Quadruple Aim, adding Clinician Experience and its importance in making decisions that impact the delivery of care. A shortfall of the initial concept was the lack of recognizing the fragmentation of workflow and decision making, as well as the lack of the clinician’s voice in the decisions that impact their ability to deliver high-quality, cost-effective care. This reinforces the idea that providers must collaborate in the decision making about care delivery.Īs many health systems embraced and implemented the concept of the Triple Aim as their framework, they may not have taken into consideration the stressful work life of clinicians and staff and how it is impacting their ability to achieve the Triple Aim goals. Today I would suggest that the Triple Aim has expanded into the Quadruple Aim, which adds the goal to improve the work life of healthcare providers. The CQO definition serves supply chain well in better understanding the concepts of the Triple Aim and to begin to clarify the aspects needed to achieve the Triple Aim. CQO looks at the intersection of, and the relationship between all costs associated with caring for individuals and communities, care aimed at achieving the best possible health and the financial results driven by exceptional patient outcomes In 2013, AHRMM responded to the Triple Aim with its Cost Quality Outcomes (CQO) movement. It is focused on improving the health of populations, improving the patient experience and reducing the per-capita cost of healthcare. To motivate MAs, we engaged them to help with model improvements and showed gratitude for all the support they provide.The Triple Aim is widely accepted as a compass to optimize health system performance. Providers were motivated to improve these communication challenges because of the benefit of the additional staffing support. As a result, we adopted “in-room documentation” as our preferred terminology. MAs had strong negative reactions to being asked to “scribe,” as that role felt demeaning.
#Quadruple aim for better administrative workflow full#
Providers struggled with allowing MAs the full time needed for the expanded rooming process, feeling the urgent need to begin the visit as soon as possible. The provider would then sigh in frustration, causing the MA to think she did her job incorrectly and then not elicit the full agenda with the next patient. For example, the MA would room the patient, elicit seven agenda items including an early refill on opiates, and relay the patient's agenda to the provider.
Leadership noted early communication issues between providers and MAs. However, in implementing and sustaining these changes, we realized we had a lot to learn about provider-staff interaction and cultural issues affecting true team-based care.

As a clinic providing integrated behavioral health care for more than 30 years, we thought of ourselves as team-based care experts. Work on communication issues (and don't call your MAs “scribes”). 5 Beyond reducing burnout, delivery models that rely on a high-functioning team have become essential given rapid increases in medical information and more prevalent chronic disease. These strategies are designed not only to reduce provider burnout but also to reduce staff burnout by ensuring that they can grow professionally and engage more intimately in patient care. To achieve the Quadruple Aim, leading primary care organizations are exploring advanced team-based strategies such as team-based documentation, previsit planning and testing, an expanded scope of practice for medical assistants (MAs) and nurses, team-based motivational interviewing and coaching, and delegation of certain elements of chronic disease care, preventive care, medication reconciliation, refills, and acute care to staff using standardized protocols. As a result of these pressures, the “Quadruple Aim,” which adds provider and staff satisfaction to the Triple Aim, has been proposed as a more sustainable approach to improving health care.


 0 kommentar(er)
0 kommentar(er)
